32yr old female was apparently asymptomatic 11 yrs ago when she (noticed yellowish discoloration of sclera and skin,) developed jaundice that susbised following medication
A similar episode occurred in 2018 which again subsided after medication
In April 2019, she developed jaundice during her 8th month of pregnancy, which resolved after being treated with medications and she had an LSCS at term.
In August 2020 she had abdominal pain for which, MRCP was performed and reported to have stone in CBD and a stricture. a stent was placed which was removed 2 1/2 momths later.
3months after stemd removal in January 2021 she underwent Cholecystectomy
She waa what is asymptomatic after cholecystectomy from January to June she had lost 9kgs, on June 7th 2021 she complaint of abdominal pain associated with vomiting with fever and chills which all lasted for one day the pain was more specific in the right hypochondrium
she had lost appetite, experienced shortness of breath and heartburn with all resolved following medication after visiting a local physician.
on 2nd July 2021 a similar episode was repeated i.e of pain in the abdomen, vomiting and fever
on 25th September, abdominal pain was unbearable which was not even control by painkillers she usually takes for pain to subside and she was admitted in AIG
on 5th October 2021 MRCP was performed a structure was noted in CHD
ercp was performed on 6th of October, she fell pain post procedure for 2 days which gradually reduced
investigations on 4/10/2021
hemogram-
hb-8.5
TLC 8800
PTS- 150,000
ESR- 34
TOTAL BILIRUBIN- 3.5
DIRECT BILIRUBIN 1.5
INDIRECT BILIRUBIN 2.0
SGPT (ALT) 93
SGOT (AST) 68
ALP 271
TOTAL PROTEINS 8.0
ALBUMIN 4.1
GLOBULIN 3.9
serim LDH- 292
Serum creatinine- 0.7
previous investigations reports:-
Radiology:-
19th August 2020
USG Abdomen IMPRESSION:
1. Hepatosplenomegaly.
Diffusely thick gall bladder with sludge and microlith
17th August 2020, USG while abdomen
Impression:-
Chronic cholecystitis with cholelithiasis. # Choledocholithiasis. # Mild splenomegaly with a hyperechoic mass in it - ? haemangioma.
1st October 2020
GALL BLADDER:
Lightly over distended gall bladder with intraluminal sludge and microliths at elongated cystic duct.
CBD is mildly dilated at porta show diffuse concentric thickening at distal segment causing mild dilatation of IHBR - benign stricture.
Mild splenomegaly.
on 20th October, 2020
IMPRESSION: MRCP reveals:
1. Hepatomegaly.
2. Over distended gall bladder.
3. Few heterogeneously enhancing iso to hyperintense lesion adjacent to head of pancreas, periceliac - Suggestive of peripancreatic
lymphnodes. callber with concentric minimally enhanc
4. Common bile duct is markedly narrowed in caliber with concentric minimally enhancing thickening of CBD wall causing minimal upstream biliary dilatation - Suggestive of benign stricture.
5. Gross splenomegaly with well defined rounded hyperintense focus within splenic parenchyma. On post contrast study minimal diffuse
30th October 2020 upper abdomen USG
IMPRESSION :
1. Mild Splenomegaly with haemangioma.
2. Mild diffuse wall thickening of Gb with calcified polyp / calculus in lumen at fundus.
3. Dilated CBD (7mm) with stent in situ.
on 15th Feb 2021 isg abdomen
IMPRESSION:
1)Post cholecystectomy status with mildly altered texture of hepatic bed at gall bladder fossa region & prominent bilobar IHBR.
2) Mildly dilated CBD with stent in situ & mild focal wall thickening at lower part
3) Normal size pancreas with heterogeneous texture.
4) Few mildly enlarged retro peritoneal lymphnodes.
5) Chronic cervicitis with PID.
5th October 2021
finding- Intrahepatic main and sectoral ducts, common hepatic duct and cystic duct remnant are dilated with abrupt cut off of common hepatic duct.
Gall bladder is not visualised History of cholecystectomy.
Mild hepatomegaly.
Small 8mm well defined hyperintensity within spleen.
Cytology study indicated- Benign Ductal Epithelial Cells. Negative for malignancy
Investigations from 9/10/2021
Hb- 8.4
TLC- 7900
Platelets- 1.9
TB- 2.21
DT - 1.23
AST- 75
ALT- 60
AKP- 594
TP- 7.2
ALB- 4.0
A/G- 1.22
She came for a follow up after and plan for further management.
hemogram-
hb-8.3
RBC- 4.20,
anisopoikiloytosis microcytic hypochromic
TLC 8500
PTS- 170,000 adequate in number, giant platelets seen
ESR- 34
TOTAL BILIRUBIN- 1.4
DIRECT BILIRUBIN 0.8
AST 46
ALP 439
TOTAL PROTEINS 6.5
ALBUMIN 3.0
A/G- 0.88
Pt underwent CBD stent removal and new stent was placed
New stent
Guide wire passed through CBD followed by CHD and left hepatic duct
Advancing stent over guide wire
Retracting the guide wire
newly placed stent
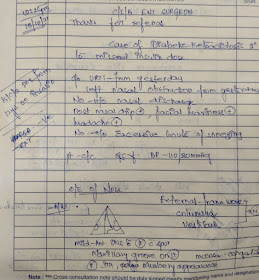
AMC Case
32 /F
Subjective-
Pt complains of 1 episode of vomiting at 5 AM, non projectile, bilious, watery, no food particles in contents
This was followed by fever sudden in onset, high grade at 5:30 AM
Objective- Patient is c/c/c
TEMP - 102.5 F
BP - 120/80 mm Hg
PR - 107 bpm
RR- 20 cpm
CVS - S1, S2 +
RS - BAE+, NVBS
P/A - soft, non tender, BS+
CNS - no FND
Assessment-Post ERCP cholangitis
(post hepatic jaundice underwent ERCP for stent replacement yesterday)
Plan-
Iv ceftriaxone
Tab paracetamol 650mg po
Tepid sponging
Laboratory investigations
Amylase 55.9
Lipase 21.3
On 30th early morning she had an episode of fever with episode of vomting associated with pain in RUQ and jaundice.
laboratory work up showed elevated TLC- 15000 and Tb- 6.0
On 31st, upon review by Gastroenterologist she developed cholangitis following which she was taken to OT and re stenting was done in KHL.