15yrs old boy was bought to the casualty with shortness of breath grade since previous night
Orthopnea+
1-2 episode of vomiting with food particles
He had similar complaints in the past( a month ago),
He was apparently asymptomatic a month back then he had 2 -3 episodes of vomiting in a day consisting of food particles and non bilious or blood stained
he had fever which subsided on medication
He complained if chest pain which was of dragging type that occured during SOB
no complaining of facial puffiness, pedal edema or reduced urine output
After consulting a physician where they incidentally found deranged renal function tests- urea 62 mg/dl
Creatinine 8.3
the following day they consulted anither physcian in Hyderabad where is RFTs further elevated-
urea- 135mg/dl and creatinine 10.7
He was suggested of Hemodialysis and proceeded with it.
he had 5 sessions in Hyderabad and 6 back at Nalgonda
USG abdomen showing B/L kidneys size of 8.1 cms Grade 3 RPD changes
Past History:
Hypertensive since 1 month and is on Tab Nicardia 10mg
History of 3 transfusions since previous month
Not a K/C/O DM ,Asthma, TB ,epilepsy ,thyroid disorders
Family History :
No H/O renal problems in their whole family
His paternal grandfather is diabetic and hypertensive
Personal History:
he is currently in 9th grade(at school)
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and Bladder movements : regular
No history of alcohol consumption, smoking or illiciting drugs
General Examination:
Patient is conscious, anxious and restless
afebrile
PR 89
BP- 130/90
RR 25
SPO2- 96
CVS- S1 S2
RS- BAE, NVBS
PA- Soft non tender
Pallor -present
Icterus -absent
Clubbing-absent
Cyanosis -absent
Generalised Lymphadenopathy-absent
Pedal Edema -absent
course of events at our hospital
soon after examining, his saturation started to reduce after which he was aided with oxygen mask
his bllop pressure began to increase which was 150/110
his blood urea was 106 and sr creatinine was 8.4
sodium 139
potassium 4.7
chloride 98
ABG on 31/10/21 at 6:30pm
pH 7.34
PCO2- 37.9
HCO3- 19.2
PO2- 62.9
SO2- 88.6
HB- 8.4
TLC- 7400
PTL- 1.6
he underwent hemodialysis last night following which hai blood pressure continued to remain elevated and his need for ixygen supply increased and was supported by BPAP
he c/o of chest pain and pain in the interscapular resion throughout the night and was too restless to sleep and was given Tramadol.
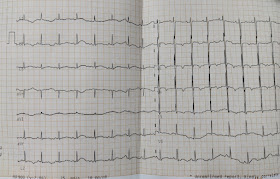
ECG AT 7:20PM (31/10/21)
ECG AT 11:20PM (31/10/21)
ECG AT 6:50 AM (1/11/21)
ECG AT 7:10 PM (1/11/21)
bedside X ray this morning at 8:30am
Repeat x ray at 11:30 AM
Considering historical presentation laboratory and radiological findings, Aortic desection and pulmonary embolism where is differential diagnosis
For a better understanding of the cause CT angiogram was planned during an attempt to shift the patient to the CT room his saturations drop from 85 to 69 and was unable to maintain saturation more than 68 in spite of being supported with bipap So he was intubated.
After intubation- E1V1M1 on inj midazolam
ACMC (PC)- Mode
FiO2- 100
PEEP 8
RR- 24
BP 130/90 on inj NORAD DS (5ml/hr)
PR- 94
RS- BAE +
coarse end inspiratory crepts were appreciated in B/L IMM, IMA ISA (R more than L)
USG chest did not suggest pleural effusion(with pressure support)
Couldn't differentiate Cardiogenic from non Cardiogenic cause
Sedation was continued with midazolam 0.4mg/kg

Bed side 2D ECHO showed Global hypokinesia
Icu - 1st bed
Day 3 of mechanical ventilation
1 session of Hemodialysis with blood transfusion done ystd , fever spikes present .
On ACMV - PC mode
With Fio2-70 % ,spo2- 100%
RR-15/ min
PEEP-6
P INSP-18cm
Vitals -
Temp -100 F
PR- 90/min , regular
BP - 130/80 mmHg
RS- BAE clear ,B/L inspiratory crepts - left more than right
CVS- S1, S2 heard .
A- Type 1 Respiratory failure - ARDS -
Hfmef ( DCMP- EF -40%)
CKD stage 5
HTN +
Plan - To wean Off from sedation
And shift to CPAP PC mode .
Treatment -
1) head end elevation 30*
2) Rt feeds
100ml milk with protein powder 4th hourly
50ml water 2nd hourly
3) Inj Meropenem 500mg Iv bd.
4) Inj Doxycycline 100mg Iv/Od
5) Inj Vancomycin 500mg iv / Bd
6)Inj pcm 1gm Iv/sos
7) Inj Lasix 40mg iv/bd
8) Tab Livogen z Rt/Od
9)Tab Bid D3 0.25mg Rt/Od
10) Tab pcm 650mg Rt/Tid
11) Neb with budecort 6th hourly
12) Chest physiotherapy
13) ET suction 6th hrly
14) change posture frequently
15) Tepid sponging /sos
16) Monitor vitals 4th hourly
17) I/O and temp charting
Icu -1st bed .
S- patient is comfortably sitting on couch ,
No shortness of breath / cough .
O- Afebrile
PR-80/min ,regular .
BP- 120/90 mmHg
RR- 28/ min
Spo2- 97% at room air
RS- BAE + clear
CVS - S1 and S2 heard
A- ARDS - cardiogenic - resolved
CKD - stage 5
HTN
P- started oral feeds .
Monitor BP .
Day 3 of vancomycin and doxy .
Day 4 of meropenam
Soap notes
Icu - first bed -
S- patient is comfortable
Conscious
Patient had one fever spike - post dailysis (103F ) , yesterday .
O- Afebrile
PR-96/ min , regular
BP-110/70 mmHg
RR-21/ min
Spo2- 97 @room air
CVS - S1 and S2 heard
P/ A - soft
CNS - NAD
A- ARDS - cardiogenic - resolved .
P- Stopped all antibiotics , monitor RR ,spo2,temp.
SOAP NOTES
12/11/21
SOAP NOTES
ICU BED 3
S- no new complaints
Objective- patient is conscious, cohorent, cooperative
afebrile
PR- 105
BP- 150/120
RR- 40 cpm
SPO2- 88% on room air
97% WITH 8L of O2
CVS- S1 S2 +
RS- BAE +
P/A- Soft non tender
A- CKD ON MHD with HTN
P- Fluid restriction less than 1.5l/day
Salt restrictions less than 2.4gm/day
Tab lasix 40 mg po/tid if spb more than 110mmhg
Tab zofer 4mg/po/tid
Tab nodosis 500mg po/bd
Tab rantac 150mg po/od
Tab nicardia 10mv po/tid
Tab met xl 50mg po/tid
Tab temla 40mg po/bd
Tab cilindipine 10mg po/od
Tab Telma 20mg po/bd
Tab livogen po/bd
Syp grylinctus 15ml po/tid
Nebulization with budecort 8th hrly
Iprevent 8th hrly
13/11/21
SOAP NOTES
ICU BED 3
S- no new complaints
Passed stools yesterday
Objective- patient is conscious, tachypnic, afebrile
PR- 94
BP- 140/110
RR- 40 cpm
SPO2- 94% WITH 15L of O2
CVS- S1 S2 +
RS- BAE + b/l inspiratory crepts+ in IAA, ISA
P/A- Soft non tender
A- CKD ON MHD with HTN
P- Fluid restriction less than 1.5l/day
Salt restrictions less than 2.4gm/day
Tab lasix 40 mg po/tid if spb more than 110mmhg
Tab zofer 4mg/po/tid
Tab nodosis 500mg po/bd
Tab rantac 150mg po/od
Tab nicardia 10mv po/tid
Tab met xl 50mg po/tid
Tab temla 40mg po/bd
Tab cilindipine 10mg po/od
Tab Telma 20mg po/bd
Tab livogen po/bd
Syp grylinctus 15ml po/tid
Nebulization with budecort 8th hrly
Iprevent 8th hrly
14/11/21
SOAP NOTES
ICU BED 3
S- no new complaints
Passed stools yesterday
Objective- patient is conscious, tachypnic, afebrile
PR- 95
BP- 110/70
RR- 18 cpm
SPO2- 100% WITH O2
CVS S1 S2 +
RS- b/l inspiratory crepts+ in IAA, IMA, Left more that R
Breath sounds reduced in SA, ISA, SSA
P/A- Soft non tender
A- CKD ON MHF with HTN
One session of dialysis was done yesterday
Cough and SOB reduced
P- Fluid restriction less than 1.5l/day
Tab lasix 40 mg po/tid if spb more than 110mmhg
Tab nicardia 10mv po/tid
Tab met xl 50mg po/tid
Tab cilindipine 10mg po/od
Tab Telma 20mg po/bd
Tab lovogen po/bd
Syp grylinctus 15ml po/tid
Nebulization with budecort 8th hrly
Iprevent 8th hrly
15YR OLD MALE PATIENT
ICU BED - 4
S - COMPLAINTS OF SOB AND CHEST PAIN
O - yesterday during dialysis patient complained of sob
O/Examination pt - conscious and tachypnic
BP : 120/70mmhg
PR : 103bpm
RR : 34 cycles
CVS : S1S2 heard
CNS : NAD
R/S : BASAL CREPTS + IN B/L IAA
P/A : SOFT , NT
A - ACUTE PULMONARY ODEMA SECONDARY TO HYPERTENSION
GLOBAL HYPOKINESIA
P - HEAD END ELEVATION
INJ. ERYTHROMYCIN 4000IU S/C WEEKLY ONCE
INJ IRON AND SUCROSE 100MG IN 100ML NS IV/BD
INJ LASIX 40MG IV/BD
TAB. CINOD 10MG PO/BD
TAB. MET-XL 20MG PO/BD
TAB TELMA 20MG PO/BD
NEB WITH BUDECORT 12TH HRLY
O2 INHALATION TO MAINTAIN SPO2
Soap notes
S-SOB (relieved) - Orthopnea (relieved)
O/Examination pt - c/c/c
BP: 110/90 mmhg
PR: 86 bpm
RR: 30 cpm
Spo2: 89% At RA.
CVS: S1S2 heard
CNS: NAD
R/S BASAL CREPTS + IN B/L IAA
P/A: SOFT, NT
A - CKD on MHD with HTN - Acute pulmonary Edema 2° to HTN ?
- Global hypokinesia
P - HEAD END ELEVATION
INJ. ERYTHROMYCIN 4000IU S/CWEEKLY ONCE 100ML NS IV/BD
INJ IRON AND SUCROSE 100MG IN INJ LASIX 40MG IV/BD TAB. MET-XL 20MG PO/BD SPO?
TAB. CINOD 10MG PO/BD
TAB TELMA 20MG PO/BD
NEB WITH BUDECORT 12TH HRLY 02 INHALATION TO MAINTAIN